Background
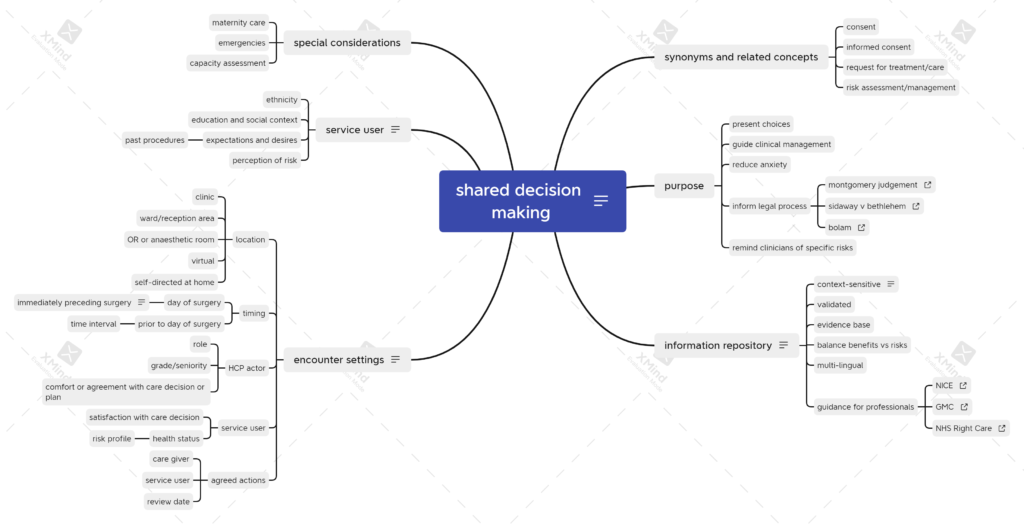
A recent project in the UK to create structured documents for shared decision making (SDM) in healthcare got me thinking about what happens in perioperative care. After gathering my thoughts in the obligatory mind map, I began to think about the differences and challenges.
The key challenge in perioperative care may be the time available for the care decision process. In the remainder of this post, I’ll focus on ways in which SDM can adapt to time constraints in a perioperative journey.
Service Users
Considering perioperative journeys, we can think of service users as falling broadly into one of three categories.
- never had surgery
- occasional surgery for unrelated conditions
- frequent flyers
For adults that had surgical procedures in early childhood, you might put them in the first category, as the procedures are unlikely to be relevant when making choices about surgery as an adult.
For adults in the second category, experience of past surgery may have an impact on present choices, but if the current procedure is unrelated to past procedures, a whole new set of choices are likely to be made.
Lastly, there is a cohort of adults that attend regularly for similar or identical procedures such as cystoscopy or other screening-type procedures. For this group, choices are generally less important, although there may be important differences in the choices of the healthcare professional (HCP) in terms of the conduct of the procedure. For example, an HCP might have a preference for general over neuraxial anaesthesia for cystoscopy. There is potential for a clash between the patient’s preferred option and that of the HCP. A key goal of the SDM process is to document and attempt to resolve these differences, recognising that there are situations where the knowledge and experience of the HCP can be the primary determinant of the choice made.
Healthcare Professionals
In addition to the biases that come with procedural experience and familiarity, HCPs also tend to focus on benefits while ignoring or understating risks and known complications. SDM tooling could (in theory) help to overcome some or all of these biases.
The seniority of the HCP is a factor. A given procedure will have a different complication rate in the hands of a more experienced operator, so this has to be factored into the SDM somehow.
Information about risks and complications should be presented in a way that is understandable and contextualised, preferably using pictures, as there is evidence that verbal descriptions of risk are widely misunderstood1.
Perhaps most important for the HCP is the time allowed for the SDM process. The subject matter for discussion may be extensive, and increases with the complexity of the procedure. For a new complex procedure with a limited amount of peer-reviewed evidence in its favour, the HCP may have a difficult task ahead of them in reaching a decision to undertake it, especially in an anxious, risk-averse service user.
To explore all the choices fully takes time, a commodity that few HCPs have in plentiful supply in their daily routine.
Brief Encounters
A well-trodden pathway for surgical pre-assessment is for a patient to have an initial telephone or video call with an HCP from a designated service, often a nurse. The practitioner usually follows a structured assessment protocol, with conditional logic to determine whether further enquiry or investigation is required. In many cases, this is the only assessment recorded before the service user attends for their procedure. There are instances when, due to administrative error, even this initial step is missed.
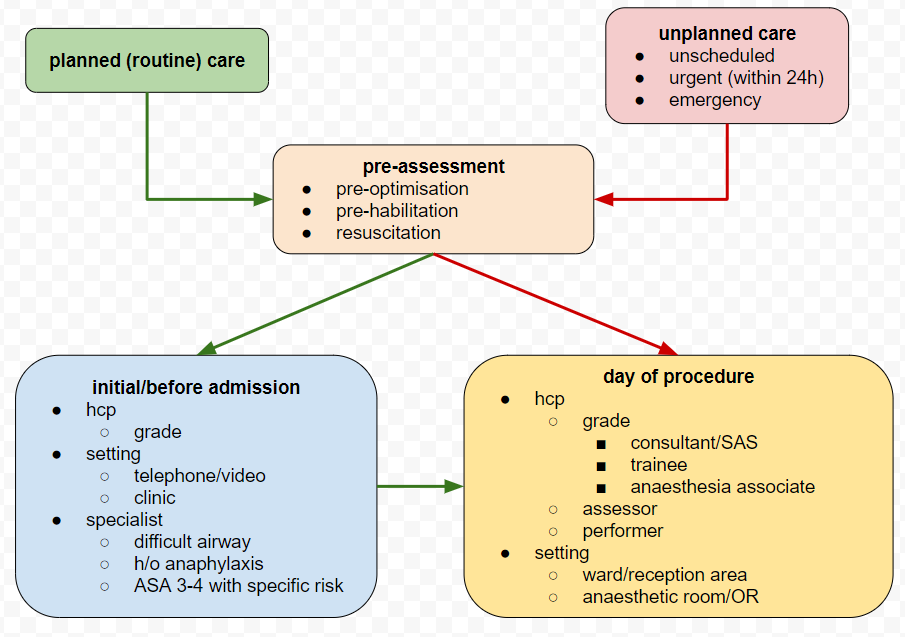
A shorter and more challenging pathway exists for urgent and emergency care, when the assessment may have to be done in parallel with initial treatment or resuscitation. In extreme cases such as emergency management of the unconscious patient, no verbal assessment is possible. Instead, the practitioner relies on any digital records that may exist and the results of physical examination.
Between these two extremes, variation is possible, but for the majority of elective (planned) surgical cases, the initial telephone or video consultation becomes a baseline assessment for the HCP responsible for care on the day of surgery. For anaesthesia in the UK, this is likely to be a consultant, SAS doctor or experienced trainee, but the immediate pre-operative visit in either the ward or reception area is often carried out by a trainee or an anaesthesia associate. Given the pressures on the surgical service, another variation is that the immediate pre-op assessment can be done by a colleague who happens to be free at the point where the patient arrives, or when an operating list crosses fixed time-period boundaries. An example is when an operating list finishes earlier than expected, a colleague can use the time for assessment of cases on other lists, even though he or she will not be involved directly in a particular list or case.
Unilateral Decision Making
Consideration must also be given to situations where a decision has to be made quickly, with or without involvement of the patient. For example, when new information or investigation results become available and the patient is under general anaesthetic or sedation. Clearly, without waking them up, by necessity any decisions made must be unilateral. A patient that lacks capacity may have an unexpected complication and there are no next of kin to contact for guidance. In these situations, a common approach is to include standard clauses for “any treatment necessary in an emergency” in the paper and (increasingly) digital consent forms that patients are asked to attest to before a procedure.
Putting all this together, it becomes evident that there are real challenges in SDM for perioperative care, with different HCPs involved at different times, and many procedures being done by staff that either haven’t met the patient before, or been involved in their care.
Meeting the Challenge
To address these issues, the anaesthesia profession in the UK have made efforts to build a common information repository for service users. The goal is to reduce both variation and wheel-reinvention by health care providers, and to give a peer-reviewed, controlled and consistent message. In addition to these digital services, traditional information leaflets are available.
As popular as they are, these digital resources have potential for improvement. Their proliferation can make the task of finding the right information for a given procedure or condition more difficult. Using internal hyperlinks within the documents can help a service user to choose between the options, but ideally, there should be a single UI that can be queried for a given procedure.
Currently, other than during assessments (remote or otherwise), there is no simple mechanism for users to ask questions of the service provider, set preferences or goals for treatment, or enter into a discussion about treatment options more generally. One can argue that this functionality sits in the domain of the personal health record, or a shared record summary, but given its importance in maximising safety and efficiency in the care pathway, efforts to design a standard for SDM become all the more exigent.
Summary
In the UK, surgical and anaesthetic services face critical pressure and their ability to deliver good outcomes is contingent on meeting the wishes and expectations of the service users through shared decision making. Digital tools such as pre-assessment pathway management, remote consultation and peer-reviewed information repositories go some way toward meeting the goal. Further progress requires a simple, intuitive interface to the user’s SDM record, so that they can confirm, edit, annotate and comment upon decisions about surgical care and anaesthetic techniques and procedures. A standard format for an SDM record would go some way towards achieving this goal, and it’s incumbent upon the profession to engage with ISOs to ensure that any proposed standard is fit for purpose.
References
1. How informed is consent? Understanding of pictorial and verbal probability information by medical inpatients
2. Assessment, Planning, Consent and Review Cycle in Perioperative Care, SCATA
